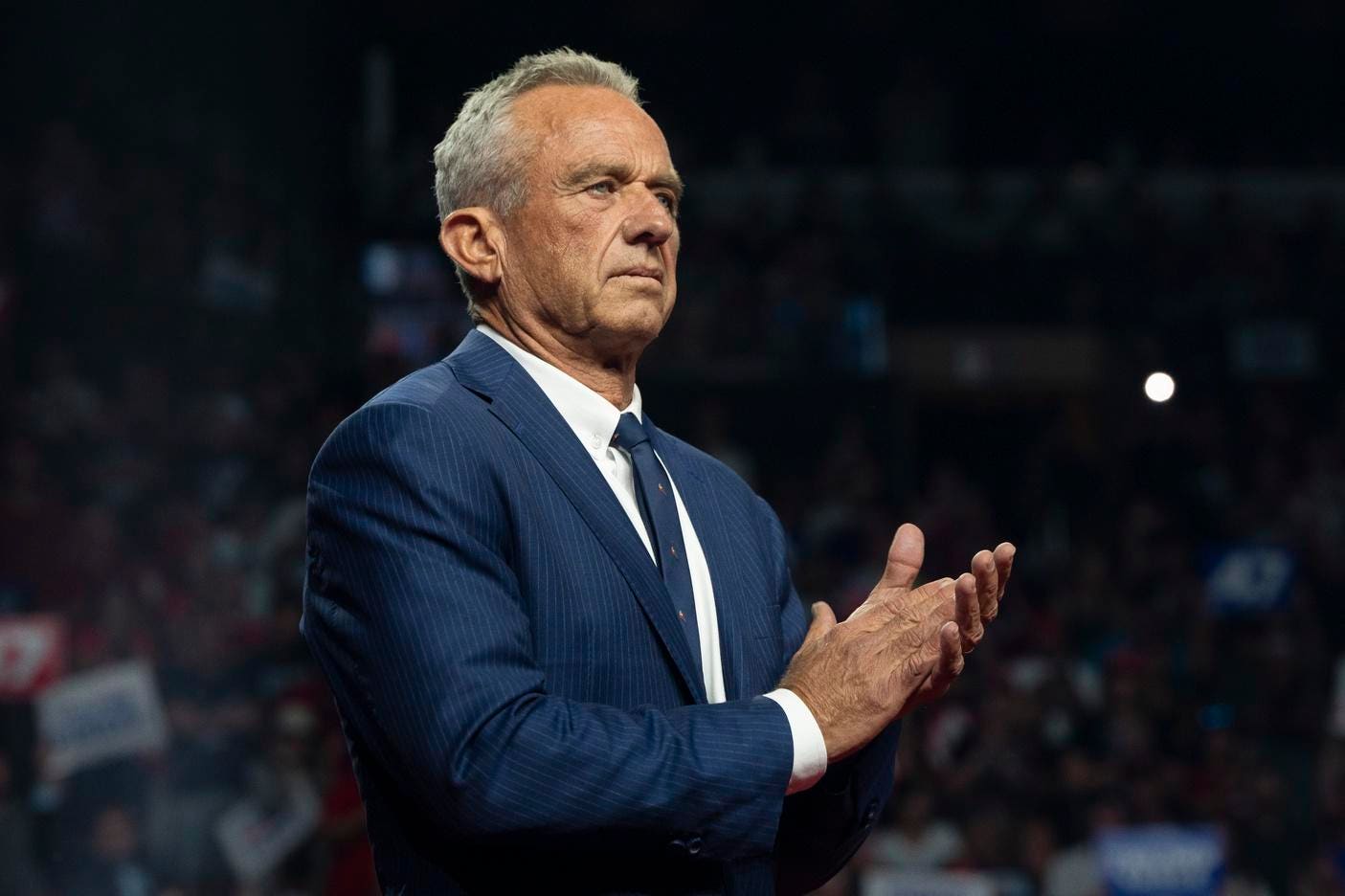
On January 7, 2026, the American landscape of public health underwent a tectonic shift that promised to redefine the relationship between the citizen, the state, and the dinner plate. At a landmark White House briefing, Health and Human Services (HHS) Secretary Robert F. Kennedy Jr. unveiled the 2025–2030 Dietary Guidelines for Americans, characterizing the move as the "most significant reset of federal nutrition policy in history." The centerpiece of this overhaul is the return of a visual icon: the Food Guide Pyramid. However, this is not the grain-heavy monument of the 1990s. The new "Real Food Pyramid" represents a total inversion of previous mandates, prioritizing metabolic health, whole-food matrices, and the aggressive elimination of industrial additives.
For more than a decade, the United States had moved away from the pyramid structure in favor of "MyPlate," a simplified graphic intended to represent a balanced meal. The 2026 return to the pyramid signifies a more prescriptive and hierarchical approach to nutrition, one that seeks to correct what current administration officials describe as forty years of "misguided, carbohydrate-dominant advice." By placing proteins and healthy fats at the foundational base of the pyramid, the federal government is signaling a departure from the low-fat, high-grain era that many critics link to the modern epidemic of metabolic dysfunction.
The Foundation: Prioritizing Protein and Lipids
The most striking feature of the 2025–2030 guidelines is the elevation of animal and high-quality plant proteins to the status of primary dietary pillars. While the 1992 pyramid relegated meat and dairy to the middle tiers and emphasized 6–11 servings of bread, cereal, and pasta at the base, the 2026 iteration places red meat, poultry, seafood, eggs, and full-fat dairy at the very bottom—the widest part of the structure.
This shift is backed by a recommendation for significantly higher protein intake: 1.2 to 1.6 grams of protein per kilogram of body weight daily. For a 180-pound adult, this translates to roughly 100 to 130 grams of protein per day, a sharp increase from the previous Recommended Dietary Allowance (RDA) of 0.8 grams per kilogram. The rationale provided by the HHS advisory council focuses on "sarcopenia prevention" and "satiety signaling." By prioritizing protein, the guidelines aim to mitigate muscle loss in an aging population while naturally reducing the overconsumption of calorie-dense, nutrient-poor snacks.
Accompanying protein at the base are "healthy fats." In a move that has already sparked intense debate within the cardiological community, the "war on fat" has been declared over. The new guidelines categorize butter, beef tallow, and full-fat yogurt alongside olive oil and avocados as foundational foods. This repositioning relies on a holistic view of food "matrices"—the idea that the health impact of a food cannot be reduced to its isolated saturated fat content. The HHS cites the PURE (Prospective Urban Rural Epidemiology) study, which followed over 135,000 participants across five continents and suggested that dairy fat consumption is associated with a lower risk of major cardiovascular events.

The Great De-Processing: Targeting UPFs and Sugars
While the promotion of fats and proteins is controversial, the secondary pillar of the new guidelines—the crusade against ultra-processed foods (UPFs)—has garnered broader support from the scientific community. For the first time, federal guidelines explicitly name and shame the "ultra-processed" category. This includes foods that undergo industrial formulations with five or more ingredients, often containing emulsifiers, thickeners, and artificial flavors.
The 2026 guidelines take a "whole-food first" approach, directing Americans to choose foods in their original, unrefined states. This policy shift is heavily influenced by a 2019 landmark study from the National Institutes of Health (NIH), which demonstrated that individuals on an ultra-processed diet consumed about 500 more calories per day than those on an unprocessed diet, despite the meals being matched for total fat, sugar, and fiber. The government’s new stance is clear: the caloric quality of a food is as important as its caloric quantity.
The "zero-tolerance" policy on added sugars is perhaps the most radical component of the reset. Previous guidelines suggested limiting added sugars to less than 10% of daily calories. The new 2025–2030 standard recommends "no added sugars" as the goal for optimal health. This creates an immediate and immense pressure on food manufacturers. In an environment where sugar is a standard preservative and flavor enhancer in everything from wheat bread to salad dressings, the federal "zero" recommendation could lead to a massive wave of product reformulations or, conversely, a surge in the use of non-nutritive sweeteners, the latter of which the guidelines also treat with skepticism.
The Microbiome and the Science of Gut Health
Reflecting the latest frontiers in biotechnology and medicine, the new pyramid introduces a dedicated emphasis on the human microbiome. The guidelines now treat the gut’s microbial ecosystem as a vital organ that must be "fed" with specific nutrients. High-fiber vegetables, low-glycemic fruits, and fermented foods—such as kefir, sauerkraut, and kimchi—are promoted as essential for maintaining an intestinal environment that suppresses systemic inflammation.
By incorporating microbiome health into federal policy, the HHS is acknowledging the growing body of evidence linking gut dysbiosis to autoimmune disorders, mental health challenges, and obesity. The advisory council noted that a diverse, fiber-rich diet is the most effective "technology" currently available for modulating human health at the cellular level. This move also includes a drastic revision of alcohol guidance. Moving away from the "moderate drinking" definitions of the past, the new guidelines state that the safest level of alcohol consumption for the microbiome and long-term health is zero, a stance that aligns the U.S. with recent health pivots in Canada and the World Health Organization.
Industry Implications and the Economic Ripple Effect
The transition from a grain-based economy to a protein- and whole-food-based nutrition policy will have profound economic consequences. The U.S. agricultural system has been optimized for decades to produce corn, soy, and wheat—the primary inputs for the very ultra-processed foods the government is now discouraging. A pivot toward "Real Food" necessitates a massive reinvestment in livestock, specialty crops (fruits and vegetables), and the infrastructure required to distribute fresh, perishable goods.

For Big Food—the multinational corporations that dominate the middle aisles of grocery stores—the 2026 guidelines represent an existential challenge. If federal nutrition programs like SNAP (Supplemental Nutrition Assistance Program) and WIC (Women, Infants, and Children) are updated to reflect these guidelines, billions of dollars in federal spending could be diverted away from processed cereals and snack foods toward fresh produce and high-quality proteins. This could trigger a "nutrition tech" boom, as companies race to develop processing methods that preserve food without the use of the "blacklisted" chemicals and sugars now targeted by the HHS.
Furthermore, the impact on the healthcare industry cannot be overstated. Current medical education in the U.S. provides notoriously little training in nutrition. The "Kennedy Reset" includes a call for the integration of metabolic health education into medical school curricula and residency programs. If physicians begin prescribing "protein and whole foods" with the same frequency as statins or insulin, the pharmaceutical industry may see a shift in demand for chronic disease management medications.
Expert Analysis and Future Trends
The reception of the new pyramid among experts remains polarized. Proponents argue that the inversion of the pyramid is a necessary "shock to the system" to halt the rising rates of Type 2 diabetes and non-alcoholic fatty liver disease. They point to the "matrix effect" of whole foods as the missing link in previous dietary advice. Critics, however, warn of the "LDL hypothesis," arguing that the promotion of red meat and saturated fats could lead to a spike in heart disease if not carefully monitored.
The nuanced cap of 10% on saturated fat—retained in the fine print of the guidelines—serves as a compromise, but the visual messaging of the pyramid clearly favors a "butter is back" narrative. This tension suggests that the next five years will be a period of intense clinical observation.
Looking forward, the "Real Food Pyramid" is likely the first step toward personalized nutrition. As wearable health tech and continuous glucose monitors (CGMs) become more mainstream, the government may eventually move toward "precision nutrition" guidelines that adapt the pyramid based on an individual’s glycemic response or genetic profile. For now, however, the 2025–2030 guidelines serve as a broad, forceful directive to the American public: return to the basics, prioritize the biological building blocks of protein and fat, and treat industrial food processing as a public health adversary.
The 2026 reset is more than a change in diet; it is a change in the American philosophy of wellness. By moving away from a model of "low-fat restriction" to one of "nutrient-dense abundance," the federal government is betting that a return to ancestral eating patterns, supported by modern metabolic science, can provide a pathway out of the nation’s current health crisis. Whether the food industry and the American palate can adapt to this radical inversion will be the defining story of public health for the next decade.