The opening weeks of 2026 have ushered in a period of intense scrutiny concerning federal health policy, culminating in the controversial release of the new Dietary Guidelines for Americans (DGA). Unveiled by the Departments of Health and Human Services (HHS) and Agriculture (USDA), these recommendations—which dictate nutritional policy across the nation, from school cafeterias to military dining halls and federal food assistance programs—have immediately ignited a firestorm within the medical and nutritional science communities. The core of the controversy centers on the guidelines’ dramatic pivot toward high-fat animal products, explicitly recommending the prominent inclusion of red meat, whole-fat dairy, and saturated fats like butter and beef tallow—a stance that directly contradicts decades of established cardiovascular epidemiology.
The DGA, a critical document updated every five years since the 1980s, traditionally relies on an exhaustive, multi-year process led by a non-partisan Dietary Guidelines Advisory Committee (DGAC). This committee comprises leading academic scientists and nutrition experts who meticulously review the latest cohort studies, clinical trials, and systematic reviews. Their findings are distilled into a comprehensive Scientific Report, which serves as the evidentiary foundation for the final federal policy. The cycle leading up to the 2026 guidelines was already underway for years, with the 2024 Scientific Report having been published on schedule. However, a significant government shutdown in 2025 delayed the final publication of the guidelines, creating an unexpected window of opportunity for political influence to reshape the final document.
When the 2026 guidelines were finally released, the disconnect between the DGAC’s scientific recommendations and the finalized policy was stark and immediate. Expectations among public health professionals included incorporating emerging data on sustainability, strengthening warnings against ultra-processed foods, and adopting the World Health Organization’s (WHO) updated stance that no level of alcohol consumption is demonstrably safe for overall health. While the new document commendably retained the foundational advice to prioritize whole foods, fresh produce, and minimize added sugars, it simultaneously introduced radical and scientifically unsupported changes regarding macronutrient composition and fat sources.
The Return of the Obsolete Pyramid
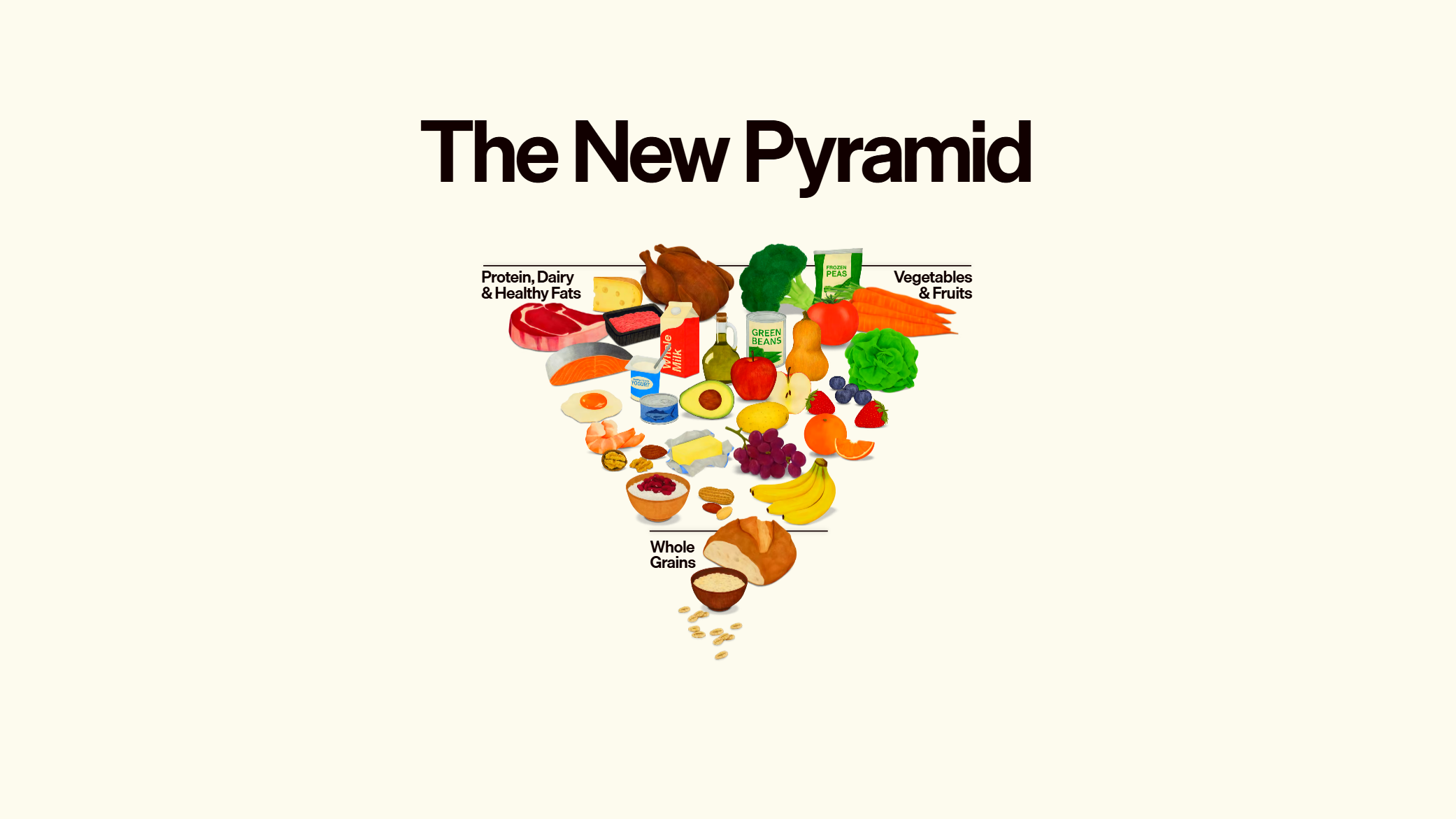
One of the most immediate visual signals of the policy shift was the adoption of an antiquated educational tool: the food pyramid. Nutrition scientists globally transitioned away from this complex, often confusing, hierarchical graphic decades ago, favoring instead the simple, proportional representation of a plate—such as the USDA’s own MyPlate model—which offers a more intuitive visual guide for meal composition.
The newly introduced "inverted triangle" is problematic not just for its obsolete format, but for its composition. The graphic prominently features a thick, seared steak and a stick of butter positioned at the apex, sharing priority space with fruits and vegetables. This visual hierarchy sends an unambiguous message: high-saturated fat animal products are foundational components of the recommended daily diet.
This prioritization clashes directly with the vast body of research linking high intake of saturated fats to elevated low-density lipoprotein (LDL) cholesterol levels, a primary risk factor for cardiovascular disease (CVD)—the leading cause of mortality in the United States. For instance, a single tablespoon of conventional olive oil contains approximately two grams of saturated fat, primarily composed of heart-healthy monounsaturated fats. In contrast, a tablespoon of beef tallow—explicitly listed as a "healthy fat" in the new guidelines—contains approximately six grams of saturated fat, while the same measure of butter yields roughly seven grams. Experts like Gabby Headrick, Associate Director of Food and Nutrition Policy at George Washington University’s Institute for Food Safety & Nutrition Security, have voiced deep concern, characterizing these endorsements as "harmful dietary recommendations" given the established lack of health-promoting benefits associated with these specific saturated fat sources at high levels of consumption.
Furthermore, the guidelines’ apparent enthusiasm for red meat disregards critical public health warnings. The WHO’s International Agency for Research on Cancer (IARC) classified red meat as “probably carcinogenic to humans” in 2015, based on evidence suggesting links to colorectal cancer. This established risk profile was wholly absent from the new federal advice, raising serious questions about the document’s commitment to evidence-based preventive health.
The Escalation of Protein Mandates
Beyond the saturated fat controversy, the new DGA proposes a dramatic increase in recommended daily protein intake. Americans are now advised to consume between 1.2 and 1.6 grams of protein per kilogram of body weight daily—a 50% to 100% increase over previous guidelines.
While adequate protein is essential for muscle synthesis and satiety, pushing consumption to these upper limits carries significant, unaddressed risks. As José Ordovás, a senior nutrition scientist at Tufts University, cautions, such an aggressive protein target invariably elevates the total caloric load and, critically, increases the intake of saturated fats and cholesterol, particularly if that protein is sourced predominantly from the favored red meat and whole-fat dairy. This metabolic strain, especially when coupled with the higher saturated fat recommendations, could exacerbate the risks for individuals already predisposed to heart disease or those with underlying kidney conditions, necessitating a highly cautious approach that the blanket recommendation fails to provide.
The advice regarding lifestyle factors was equally problematic in its vagueness. While the guidelines mentioned consuming "less alcohol for better overall health," this provides zero actionable guidance for consumers, particularly in light of recent research suggesting that the long-held concept of a "safe" threshold for alcohol consumption is scientifically untenable. Similarly, while highly processed foods were generally discouraged, the document failed to adopt a clear, scientifically validated definition of "ultra-processed," undermining the enforceability and educational utility of the warning.

The Crisis of Opaque Governance
The scientific community’s profound disappointment stems less from the specific recommendations and more from the apparent political interference that bypassed established, transparent scientific review processes. Multiple contributors to the previous guidelines and researchers involved in drafting the 2024 Scientific Report refused to comment publicly, yet conveyed strong feelings of disgruntlement and frustration, noting that the process by which the final 2026 guidelines were assembled was "opaque."
The established DGA framework is designed to insulate public health advice from political and commercial pressures. The DGAC spends years synthesizing data, receiving public comment, and vetting findings. The final guidelines, however, are ultimately policy documents signed off by the Secretaries of HHS and USDA. The decision to discard the DGAC’s carefully vetted conclusions—which presumably included adherence to cardiovascular risk mitigation strategies—in favor of recommendations championed by powerful industry groups represents a significant erosion of scientific integrity. This move signals that political appointees prioritized specific agricultural interests over the consensus findings of nutritional science experts, converting a public health document into an economic mandate.
As Ordovás observed, the DGAC members invested years of meticulous work identifying and synthesizing relevant scientific studies. Seeing that thorough, peer-reviewed effort discarded and replaced by quickly assembled, contradictory material generates not just professional disappointment, but a deep crisis of confidence in the federal government’s ability to provide unbiased health guidance.
Industry Implications and Market Shifts
The ripple effects of the 2026 DGA are projected to be substantial, particularly within the agricultural and food technology sectors.
For the conventional meat and dairy industries, the guidelines represent a major political and economic victory. The elevation of steak, butter, and tallow to "healthy" status serves as a powerful federal endorsement, potentially stabilizing or increasing consumer demand for these products, which have faced decades of pressure due to health and environmental concerns. This victory validates the aggressive lobbying efforts often deployed by commodity groups in Washington, ensuring favorable policy outcomes within the USDA’s purview.
Conversely, the plant-based and alternative protein sectors face an unexpected headwind. Companies developing lab-grown meat, plant-based dairy substitutes, and innovative fat alternatives rely on a public health environment that encourages reducing high-impact, high-saturated fat animal products. The 2026 DGA undermines this narrative, potentially slowing market adoption and making it harder for these emerging technologies to compete for federal procurement contracts (e.g., in school lunch programs) where compliance with DGA recommendations is mandatory.
In the realm of public health policy, the implementation challenges are severe. Federal programs like the Supplemental Nutrition Assistance Program (SNAP) and the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) use the DGA to structure eligibility and recommended food lists. Implementing guidelines that promote high saturated fat intake while simultaneously attempting to address soaring rates of obesity, type 2 diabetes, and cardiovascular disease creates a logistical and ethical contradiction for public health administrators and frontline nutritionists.
Future Impact: The Politicization of the Plate
The ultimate impact of the 2026 Dietary Guidelines transcends mere dietary advice; it challenges the foundational role of science in public policy. By overriding the DGAC, the administration has set a dangerous precedent, suggesting that national health mandates are susceptible to political and economic pressure, rather than being grounded solely in the best available evidence.
This politicization threatens to deepen public distrust in federal institutions, forcing individuals to navigate contradictory information from their government and their healthcare providers. When the scientific process is perceived as "opaque" and the findings of established experts are ignored, the public is left confused, making informed dietary choices significantly more difficult.
Moving forward, the scientific community must redouble efforts to conduct robust, independent research, perhaps seeking alternative, non-governmental channels to disseminate unbiased, evidence-based nutritional recommendations. The episode serves as a stark warning: safeguarding the integrity of public health guidelines requires vigilance against the pervasive influence of special interests and a steadfast commitment to scientific transparency, lest the nation’s diet be determined by political mandate rather than medical consensus. The next five years will be a crucial test of whether America’s public health infrastructure can effectively mitigate the risks inherent in the federal government’s current, scientifically questionable nutrition strategy.