The scale of the cybersecurity incident impacting Covenant Health, a significant healthcare provider serving communities across New England and parts of Pennsylvania, has dramatically expanded following rigorous post-incident forensic analysis. What began as an initial disclosure in July reporting the exposure of just under 8,000 patient records has now been revised to encompass the sensitive information of 478,188 individuals. This substantial recalculation—nearly sixty times the original figure—underscores the protracted and often underestimated complexity involved in accurately quantifying the fallout from major ransomware attacks targeting large, interconnected healthcare ecosystems. Covenant Health, headquartered in Andover, Massachusetts, manages an array of facilities including hospitals, specialized rehabilitation centers, assisted living residences, and elder care organizations, making the sensitivity and breadth of the compromised data particularly concerning for regional patient privacy.
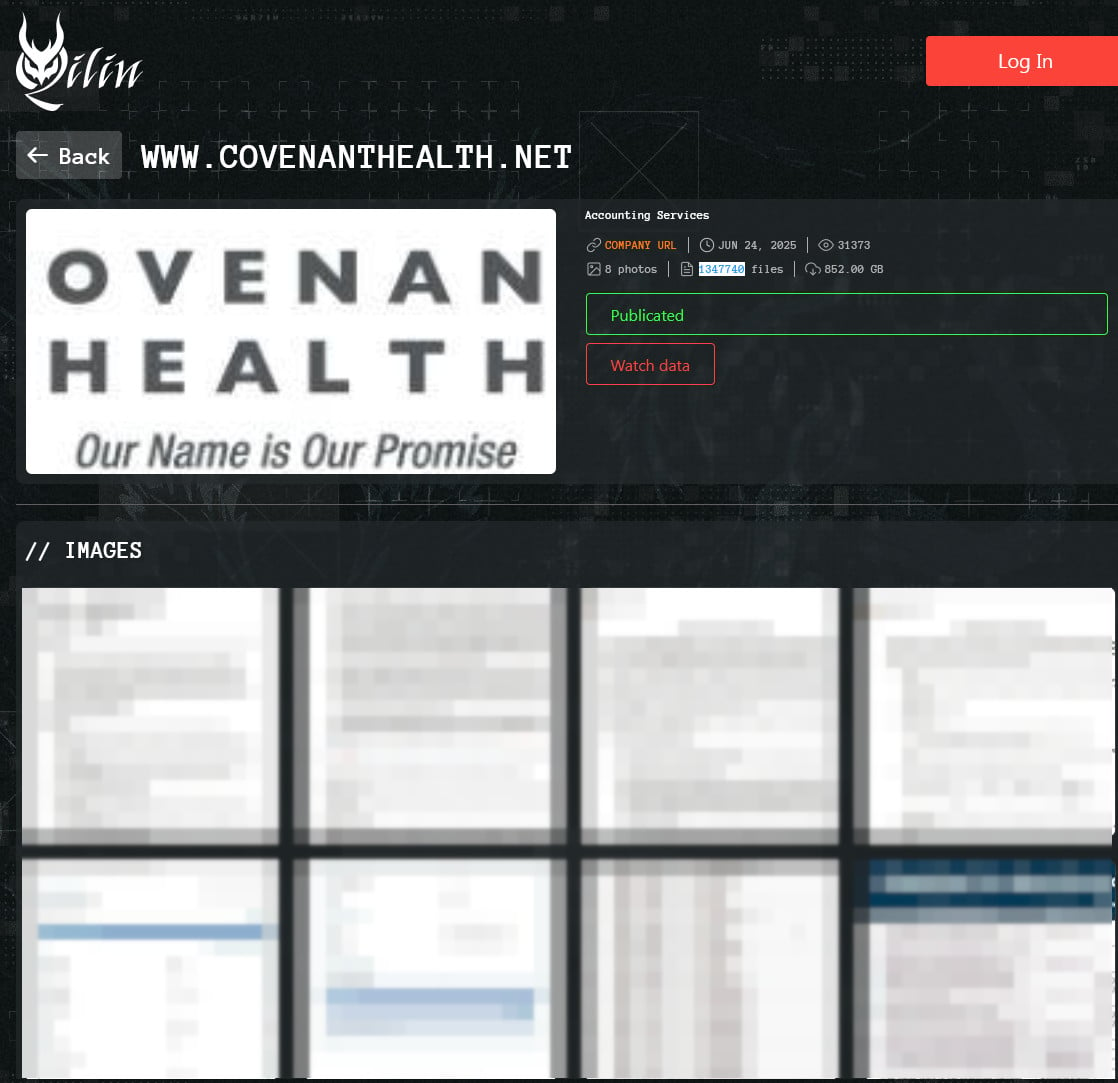
The initial discovery of the breach occurred on May 26, 2025, with internal systems flagging unauthorized access that investigation traced back to May 18, 2025. This eight-day window provided attackers ample opportunity to traverse the network and exfiltrate data before the intrusion was contained. The narrative surrounding this event gained international attention when the Qilin ransomware syndicate publicly claimed responsibility in late June. Qilin’s typical modus operandi involves double extortion—encrypting systems to disrupt operations and simultaneously stealing data to threaten public release. The group boasted of securing a massive trove: 852 gigabytes of data, cataloged as nearly 1.35 million distinct files, pointing toward a deep compromise of Covenant Health’s data repositories.
The nature of the compromised data elevates this incident beyond a mere operational disruption into a significant threat vector for identity theft and medical fraud. According to Covenant Health’s official notifications, the exposed information is highly granular and deeply personal. It includes standard personally identifiable information (PII) such as names, residential addresses, dates of birth, and critical identifiers like medical record numbers and Social Security numbers. Crucially, the breach also compromised protected health information (PHI), detailing health insurance specifics, diagnoses, records of treatment received, and the specific dates associated with those medical interventions. For nearly half a million people, the digital safety net has been severely compromised, potentially exposing them to tailored phishing attacks or long-term financial exploitation.
Covenant Health’s response mechanism involved immediately engaging specialized, third-party forensic investigators to meticulously parse the evidence and map the exact scope of the exfiltration. The disparity between the initial report (7,864 patients) and the final tally (478,188 patients) highlights a common pitfall in breach response: underestimation based on preliminary log analysis or limited scope containment. Often, initial findings only capture data accessed from the first point of entry, while comprehensive deep-dive forensics are required to uncover lateral movement and access to less obvious, yet highly sensitive, data backups or archival systems. The ongoing nature of this review, even months after the initial detection, emphasizes that data mapping in sprawling IT environments is never instantaneous.

In recognition of the severity, Covenant Health has initiated mandatory notification procedures, beginning mailing detailed breach notification letters to affected parties starting December 31st. Furthermore, as a standard remediation measure in high-stakes data compromises, the organization is extending 12 months of complimentary identity protection and credit monitoring services to all impacted individuals. While these services offer a necessary layer of mitigation against immediate misuse, cybersecurity experts often caution that the value of SSNs and comprehensive medical histories often far exceeds the one-year coverage period offered post-breach.
Industry Implications: The Growing Target Profile of Healthcare
This incident involving Covenant Health serves as a potent case study illustrating the persistently high-risk environment enveloping the U.S. healthcare sector. Healthcare organizations are increasingly becoming prime targets for sophisticated cybercriminal syndicates like Qilin not just because they possess vast amounts of data, but because the data’s utility for extortion is higher. Unlike financial data, which can be rapidly canceled or replaced, health records are immutable—a patient’s diagnosis or SSN remains constant, offering lifelong value on dark web marketplaces for insurance fraud, prescription drug diversion, and targeted blackmail.
The complexity of healthcare IT infrastructure exacerbates this vulnerability. Organizations like Covenant Health operate a heterogeneous environment, mixing legacy Electronic Health Record (EHR) systems with modern cloud services, specialized medical imaging equipment (PACS), and various Internet of Medical Things (IoMT) devices. Each integration point represents a potential unpatched vulnerability or an overlooked configuration error that sophisticated actors can leverage for initial access or persistence. The initial breach in May suggests a successful compromise of core network infrastructure, which subsequently allowed Qilin to probe deeper into areas containing aggregated patient databases.
Furthermore, the healthcare industry often grapples with balancing stringent patient care demands against necessary security investment. In high-stakes environments where uptime equates directly to patient safety, security protocols that might cause even momentary service interruption—such as rigorous access controls, mandatory multi-factor authentication across all legacy endpoints, or aggressive network segmentation—are sometimes circumvented or poorly enforced to maintain clinical flow. This tension creates an operational risk environment that cyber adversaries are adept at exploiting.
Expert Analysis: The Forensics Gap and Disclosure Timelines
From a forensic and regulatory perspective, the timeline of disclosure warrants critical analysis. The gap between the incident date (May 18) and the initial report (July) reflects the necessary triage and initial investigation phase. However, the subsequent revision from 7,864 to 478,188 individuals months later points toward challenges in scope definition. Expert security architects emphasize that defining "impacted" often involves more than just identifying which database was queried. It requires tracing data lineage—determining if data was merely viewed, copied, or exfiltrated, and cross-referencing these events against data retention policies and access logs across disparate systems.
The Qilin group’s specific claim regarding 1.35 million files is noteworthy. In many breaches, the file count claimed by threat actors slightly inflates the actual number of unique, high-value records, often counting system logs or non-patient-specific administrative files. The forensic team’s final count of 478,188 individuals suggests a more precise, verified enumeration of records containing sensitive PII/PHI, indicating a successful, albeit delayed, reconciliation between the attacker’s narrative and the organization’s verified findings.
Regulators, particularly those overseeing HIPAA compliance in the U.S., place significant weight on the thoroughness and timeliness of the investigation. While immediate containment is paramount, the ability to accurately quantify the harm done is essential for determining appropriate mitigation steps and potential penalties. This incident underscores the need for healthcare organizations to invest in continuous monitoring solutions that provide immutable audit trails, allowing for faster, more granular scoping during a crisis, rather than relying solely on post-incident retrospective analysis.
Future Impact and Trends in Healthcare Cyber Resilience
The Covenant Health breach is symptomatic of several escalating trends that will define the cybersecurity landscape for the healthcare sector moving forward.
1. Ransomware Targeting Specificity: Threat groups are moving beyond opportunistic attacks toward highly targeted campaigns against organizations with critical infrastructure and high-value data. Qilin’s focus on a mid-to-large regional provider suggests a calculated decision that the ransom yield from healthcare operations will likely outweigh the risk of law enforcement disruption.
2. The Data Lifecycle Management Imperative: Future resilience hinges on rigorous data lifecycle management. If Covenant Health had implemented stricter, automated controls over the retention of highly sensitive identifiers (like SSNs) or segmented PHI more aggressively, the impact of a perimeter breach could have been significantly curtailed. Organizations must adopt a "zero trust" philosophy not just for network access, but for data access, assuming that once an attacker is inside, they will seek the crown jewels.
3. Regulatory Scrutiny on Vendor Management: As healthcare providers rely heavily on third-party software, cloud hosting, and outsourced IT services, the regulatory focus is increasingly shifting toward supply chain risk. A breach often originates not in the core hospital system, but through a less secure connection to a billing partner, a remote diagnostic service, or a managed security provider. Comprehensive auditing of vendor security postures will become mandatory, not optional.
4. The Shift to Proactive Defense: The industry must move decisively away from reactive remediation, which often involves lengthy forensic investigations and public relations crises, toward proactive, continuous risk posture management. This includes adopting advanced techniques like attack surface management (ASM) to continuously map external and internal digital exposures, ensuring that systems strengthened post-breach remain fortified against the next wave of evolving threats. Covenant Health’s statement about strengthening security is standard, but the true measure of success will be their ability to demonstrate measurable, sustained improvements in areas like vulnerability patching cadence and endpoint detection and response (EDR) efficacy in the coming fiscal year.
The fallout for Covenant Health involves not only significant financial costs associated with remediation, legal fees, and credit monitoring, but also the intangible, yet critical, erosion of patient trust. In the healthcare sector, where confidentiality is a fundamental component of the provider-patient relationship, a breach affecting nearly half a million individuals necessitates a sustained, transparent commitment to rebuilding that confidence through demonstrable, verifiable security enhancements. The revised figures confirm that this incident is one of the most significant healthcare data compromises of the year, serving as a stark warning across the industry about the pervasive and growing threat posed by organized cybercrime against patient welfare.

