The initial stages of human conception—the delicate dance where a nascent life form establishes its tenure within the maternal environment—constitute one of biology’s most profoundly consequential yet historically obscured processes. What unfolds at this critical juncture, known as implantation, is the true commencement of gestation: a spherical, pre-embryonic structure, the blastocyst, initiates physical contact with the highly specialized lining of the uterus, the endometrium, securing its position and beginning the formation of the vital placental interface.
Yet, this foundational moment, which determines the success or failure of a pregnancy, has always been hidden from direct observation, occurring deep within the biological confines of the human body. Groundbreaking new work, however, is now illuminating this dark phase of development by recreating the implantation environment in vitro. A collaboration of international research teams, notably including efforts originating in Beijing, as well as joint projects spanning the United Kingdom, Spain, and the US, have recently detailed in a series of publications the most sophisticated models yet of early human implantation, achieved by integrating human embryos or their stem-cell mimics with bioengineered tissue structures known as organoids.
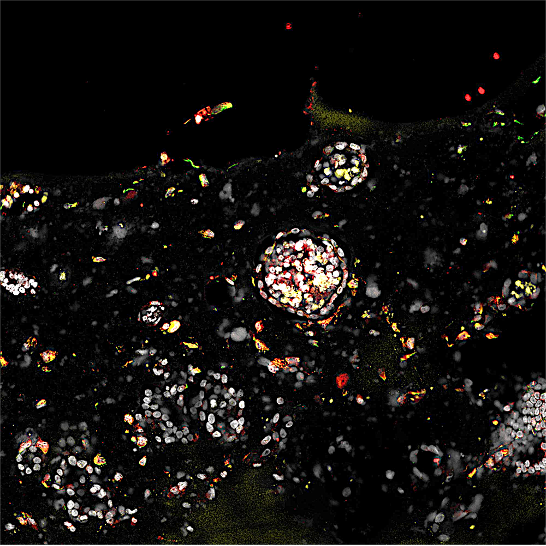
These three-dimensional constructs represent a technological leap, moving beyond traditional two-dimensional cell cultures. Scientists have cultured endometrial cells—the very tissue that lines the uterus—to form complex, functional organoids. These micro-uterus models are housed within bespoke microfluidic chips, transparent silicone chambers engineered with microscopic channels to facilitate nutrient delivery and waste removal, closely mimicking the dynamic physiological conditions of the native environment. This innovative platform allows researchers unprecedented, real-time visualization of the embryonic-maternal cross-talk.
Jun Wu, a prominent biologist affiliated with the University of Texas Southwestern Medical Center who contributed to the Chinese studies, underscored the technological confluence driving this advance. "The fundamental innovation across all three reports is the successful co-culture of the human embryo and the functional endometrial organoid," Wu stated. This union allows for the meticulous dissection of the molecular and mechanical signals exchanged between the developing organism and the receptive maternal tissue—a dialogue that has remained a scientific black box until now.
The 14-Day Boundary and the Implantation Bottleneck
The ability to maintain these integrated systems is currently curtailed by well-established ethical and legal frameworks. In nearly all jurisdictions globally, research involving intact human embryos is strictly limited by the "14-day rule," or the appearance of the primitive streak, whichever comes first. This boundary dictates that the experiments detailed in the recent publications were halted when the embryos reached two weeks of development, ensuring compliance with established international bioethical norms regarding the complexity of the developing human nervous system.
Understanding implantation is not merely an academic exercise; it addresses the most persistent clinical bottleneck in assisted reproductive technology (ART). The cornerstone procedure, in vitro fertilization (IVF), involves external fertilization followed by several days of laboratory culture until the embryo reaches the blastocyst stage. This blastocyst is then transferred to the patient’s uterus. Despite decades of refinement, IVF success rates remain modest, largely because the majority of cycles fail at the point of transfer—the embryo simply fails to attach and establish viability.
Matteo Molè, a Stanford University biologist whose research contributed to the multi-national paper, highlighted the shift in focus. "IVF traditionally focuses on the in vitro fertilization phase. What we have now achieved is the stage of in vitro implantation," Molè explained. "Given that implantation is the primary barrier to successful pregnancy outcomes, mastering its modeling in the laboratory holds immense potential for significantly boosting clinical success rates."
For years, developmental biologists like Hongmei Wang, a co-leader of the Beijing Institute for Stem Cell and Regenerative Medicine effort, relied on primate models to gain any insight into this developmental period, often requiring invasive interruption of pregnancy to harvest tissues. "We have always recognized the importance of studying human embryo implantation, but the sheer lack of visibility, due to it occurring entirely within the uterus, meant we lacked a way to do so," Wang observed. The microfluidic organoid system provides the necessary window, offering a high-resolution view previously impossible in human systems.
Leveraging Synthetic Embryo Models for Scale
A key component of the research, particularly in the Beijing study, involved the strategic use of blastoids. While a limited number (approximately 50) of donated IVF-derived human embryos were tested, the bulk of the experimentation—over a thousand trials—utilized these synthetic counterparts. Blastoids are structures derived from pluripotent stem cells that self-assemble into entities closely mimicking the architecture and cellular composition of a natural blastocyst, though they are not considered true embryos and possess no potential for full development.

This distinction is crucial for scaling up research. As Leqian Yu, the senior author from the Beijing Institute, noted, "The fundamental question became, how do we operationalize these blastoids? The obvious next application was implantation modeling." Because blastoids circumvent many of the stringent ethical and regulatory hurdles associated with using genuine human embryos, they can be manufactured in large numbers and deployed for high-throughput screening and optimization studies.
The design of the Beijing team’s microfluidic chamber was instrumental in achieving successful implantation simulation. It comprised a specialized silicone matrix, carefully engineered to possess the mechanical softness necessary for tissue growth, incorporating internal channels for continuous perfusion of specialized culture medium. This highly controlled environment provided the ideal substrate for the endometrial organoid, allowing researchers to introduce either blastoids or real blastocysts through a defined access window, initiating the simulated "pregnancy."
Yu emphasized the profound nature of the observation capabilities this technology affords: "We sought to identify the first instances of cross-talk—the signaling mechanisms between the embryo and the maternal tissue. I believe this marks the first time we can observe this entire early process unfold dynamically."
Industry Implications and the Dawn of Precision Fertility
The immediate industry implications of these organoid-based models are transforming the landscape of reproductive medicine. The commercial sector is rapidly moving to translate this laboratory capability into clinical tools, signaling a broader trend toward personalized fertility treatments, often referred to as "precision fertility."
Startups such as Dawn Bio (based in Vienna) and Simbryo Technologies (Houston) are capitalizing on this technology. Simbryo, for example, has announced plans to offer personalized prediction services for IVF patients. This involves a crucial shift in diagnostic methodology: instead of relying on generalized population data or basic hormone measurements, the approach is highly patient-specific.
The diagnostic process begins with a minor biopsy of the patient’s own uterine lining. Cells harvested from this biopsy are then cultured to generate personalized endometrial organoids. These patient-derived models are subsequently exposed to blastoids. The ensuing interaction is used as a predictive assay: if the blastoids fail to successfully initiate implantation and attachment into the patient’s organoid, it strongly suggests that the patient’s uterus is biologically unreceptive, potentially identifying the root cause of repeated, unexplained IVF failures. This approach moves the assessment of uterine receptivity from theoretical timing calculations to empirical, functional validation.
Beyond prediction, the organoid platform is proving invaluable for therapeutic discovery. The Beijing team applied their system to tissue derived from women with documented histories of recurrent implantation failure (RIF). Utilizing the blastoid-organoid model, they performed high-throughput screening against an extensive library of 1,119 previously approved drugs. The objective was to identify existing pharmaceutical agents that could enhance endometrial receptivity.
The screening yielded several promising candidates. Most notably, avobenzone—a chemical commonly utilized as a UV filter in various sunscreens—demonstrated a remarkable capacity to increase the implantation success rate of blastoids, elevating the attachment frequency from a baseline of just 5% to approximately 25% within the RIF-derived organoids. This discovery underscores the utility of the platform for drug repurposing, offering a faster route to potential clinical trials than developing novel compounds. The research team intends to pursue rigorous preclinical validation and hopes to launch a clinical trial based on the most efficacious and safe drug candidates identified through this system.
Expert Analysis: The Complexity of Ectogenesis
The success of these models immediately raises profound questions regarding the future trajectory of developmental biology and the concept of ectogenesis—the development of an organism entirely outside of the maternal body. While the current organoid models are revolutionary, they remain simplified systems, lacking the full complexity of a native uterus.
The current technical limitations are well-recognized by the researchers. The organoids lack critical components, including a functioning microvasculature (blood supply) and essential immune cell populations. The native uterus is not merely a passive receptacle; it is a highly vascularized, immunologically active site where maternal immune cells actively modulate the implantation process, protecting the mother while tolerating the semi-allogeneic fetal tissue.

To advance the fidelity of the model, researchers are focused on engineering circulatory systems. Yu’s team in Beijing, for instance, is actively working to integrate blood vessels and microscopic pumps into their chip device, aiming to create a rudimentary, continuous circulation for the organoids.
Should these bioengineering challenges be overcome, the capacity to grow blastoids or genuine embryos for longer periods will become a reality, pushing the boundaries of the 14-day rule. Jun Wu acknowledges this trajectory: "This technology is fundamentally related to ectogenesis. It inevitably raises the possibility of extending gestation ex vivo."
However, Wu maintains a cautious perspective regarding the immediate future. Incubating a human fetus to full term in a laboratory—creating a complete artificial womb—requires overcoming challenges that remain squarely within the realm of science fiction, for now. Full ectogenesis requires simulating the complex physiological and hormonal feedback loops, the nutritional delivery, waste processing, and mechanical support systems of the placenta and amniotic sac, all in continuous, coordinated action for nine months. Current research, while impressive, only replicates the first few days of this intricate process.
The immediate and ethical focus of this research remains firmly fixed on enhancing clinical outcomes for infertility patients and unlocking the fundamental mysteries of early human development. By visualizing and manipulating the implantation phase, scientists are gaining the tools necessary to refine IVF protocols, screen for effective therapeutics, and ultimately, personalize reproductive care with unprecedented precision, moving beyond the historical guesswork that has long characterized the treatment of implantation failure. The true value of these bioengineered uterine models lies not in creating artificial babies, but in giving researchers the key to decoding the most vital, yet most hidden, chapters of human biology.
Future Trends: The Pressure on the 14-Day Rule
The technological advances demonstrated by these co-culture systems intensify the ongoing global debate surrounding the ethical constraints of the 14-day rule. Historically, this limit was set because beyond this stage, human embryos become increasingly difficult to study in vitro using traditional methods, and because the primitive streak—the first morphological sign of the establishment of the body axis—appears around this time, signaling the onset of genuine individual development.
With the advent of sophisticated organoid and microfluidic technology, the technical feasibility of maintaining an integrated embryo-endometrial unit beyond two weeks is rapidly approaching. This raises significant ethical pressure. If scientists can sustain development to Day 20 or Day 28—the period where major organ systems begin to differentiate and the true foundations of the central nervous system are laid—the rationale for stopping at Day 14, purely due to technical difficulty, evaporates.
Policymakers and bioethicists are already engaged in discussions about potentially extending the research limit, perhaps to a "28-day rule," provided that robust oversight and compelling scientific justifications (such as studying the origins of miscarriage or congenital defects) are in place. The data generated from these new organoid models will be critical evidence in these deliberations, as they provide tangible proof of what can be learned about human developmental pathology during the currently prohibited window.
Ultimately, the confluence of stem cell technology, microfluidics, and tissue engineering is rapidly redefining the boundaries of reproductive science. These laboratory models are poised to revolutionize how we diagnose infertility, screen for developmental disorders, and potentially even prevent early pregnancy loss, shifting the focus of reproductive medicine from generalized statistical success to individualized biological certainty. The age of precision reproductive medicine, powered by bioengineered models, is now underway.